You’re knee-deep in building a telehealth platform, or a patient portal, or some slick backend service that talks to EHRs. The code’s looking good, the UI is snappy, and you’re feeling pretty proud. Then someone drops the H-word: HIPAA. And suddenly, your brain goes quiet. Like when your laptop fan kicks on during an awkward silence.
Contents:
As developers and product folks, we’re wired to solve problems, ship features, and make things work. Compliance stuff feels like paperwork hell because you don’t want to mess up people’s medical data. You can easily get fined or damage your brand reputation.
This article aims to give you practical guidance on HIPAA compliance for software development that respects patient privacy without grinding your dev cycle to a halt. Stick around to learn all the essentials like—What actually counts as ePHI? When do you need a BAA? How to design auth flows that won’t make a compliance officer cry?
What is HIPAA Compliance For Software Development?
It means building systems that protect patients’ health information by design. That includes how you store it, who can access it, how you track changes, and what happens if something goes wrong.
HIPAA (Health Insurance Portability and Accountability Act) was passed in 1996. Yeah, pre-smartphone era. So the law itself doesn’t really relate to using OAuth or encrypting all API responses. What it does do is set expectations: if your software handles protected health information (PHI), you have to keep it secure, private, and accountable.
And here’s where things get real for us devs and product folks: if your app touches PHI, even indirectly, you’re part of the chain of responsibility.
So what counts as PHI? Well, anything that can identify a patient and relates to their health status, care, or payment. The list is longer than you think—18 identifiers, to be exact—and once any one of them gets mixed with health data, boom: HIPAA software compliance applies.
Now, I know what some of you are thinking: “But we’re just a SaaS tool! We don’t treat patients!” Doesn’t matter.
If you’re storing, transmitting, or processing PHI, even as a third-party vendor, you’re likely considered a Business Associate under HIPAA. That means you need a Business Associate Agreement (BAA) with the covered entity, like a hospital or clinic, and you’ve got to follow the rules.
Which brings us to the actual meat: the Security Rule. This is the part that matters most for software teams. It breaks down into three buckets:
- Administrative safeguards: Stuff like risk assessments, employee training, and assigning a privacy officer.
- Physical safeguards: Mostly about where servers live, device access, etc. If you’re using AWS or Azure and not doing anything weird, cloud providers cover a lot.
- Technical safeguards: Now we’re talking your turf. Authentication, encryption (both in transit and at rest), audit logging, role-based access control, etc. This is where your architecture decisions either save the day or come back to bite you.
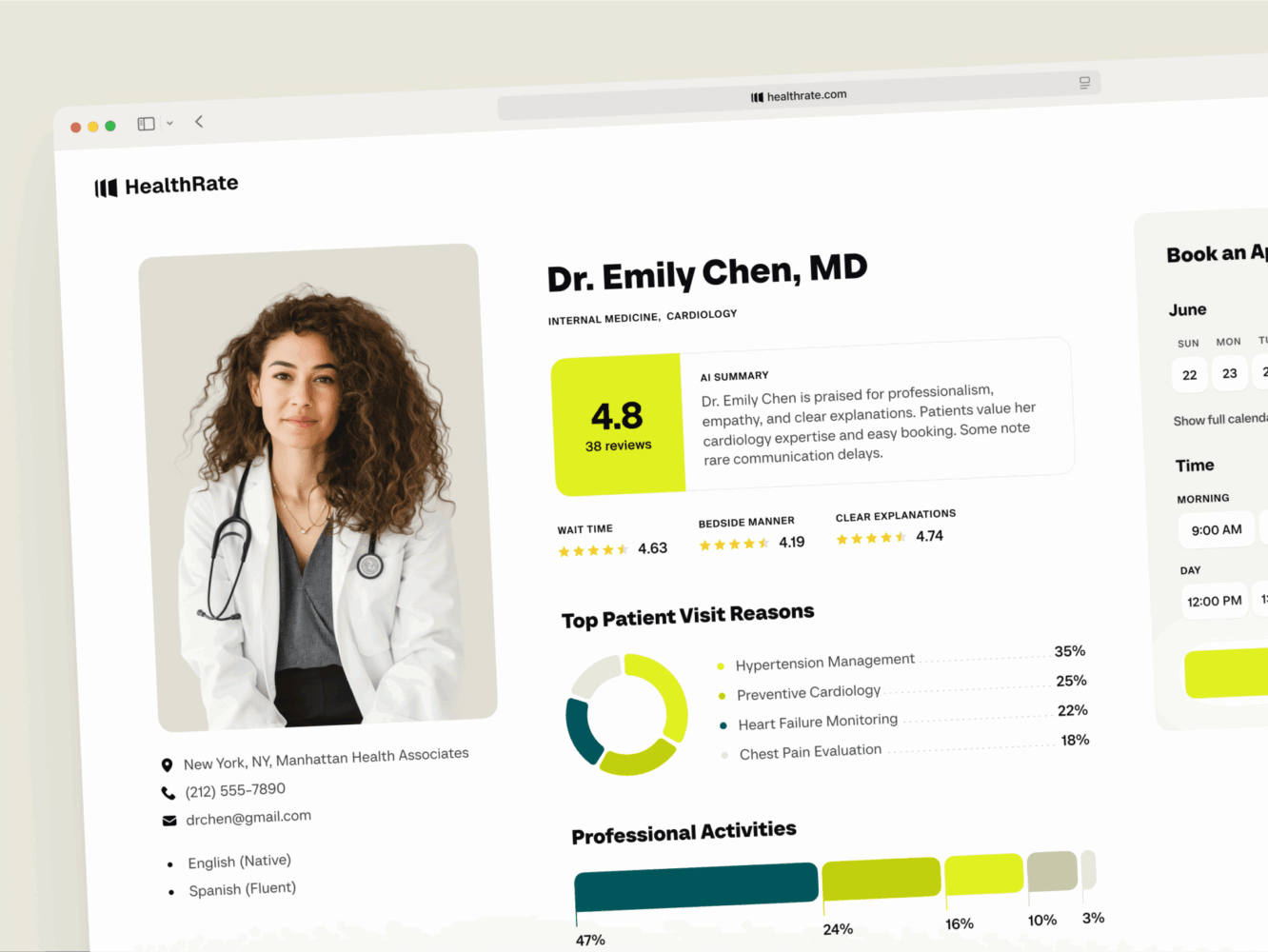
Design for Healthcare Platform by Conceptzilla
HIPAA IT Compliance Checklist for Software Developers
We know what the stuff really is, but how can you notice that your product falls under its influence, and what should you do? Well, here are a few steps:
✅ First, answer: Are you touching PHI?
Are you storing, transmitting, or processing any health data tied to an individual? Even indirectly (like syncing with an EHR)? Even if it’s “just for analytics”?
If the answer is yes, then HIPAA likely applies. If the answer is maybe, treat it as yes until a lawyer advises otherwise. Just because you don’t see the full record doesn’t mean you’re off the hook. Hashed emails and diagnosis codes? Still PHI.
✅ Sign that BAA (Business Associate Agreement)
Just paperwork, but it matters. If you’re working with a hospital, clinic, or health tech platform, get a signed BAA before exchanging any data. And no, a Terms of Service click-wrap doesn’t count.
✅ Encrypt the right things, both at rest and in transit
Also:
- Data at rest, such as PHI in databases, backups, and logs, must be encrypted. AES-256 is your friend.
- Use managed key services (like AWS KMS, Azure Key Vault). Don’t roll your own crypto.
- Don’t forget temporary files, cache layers, or staging environments.
- Enable HTTPS by default, redirect HTTP and set HSTS headers.
✅ 4. Lock down access (RBAC + MFA)
Who can see what? You need to implement role-based access control where doctors see more than billing staff, and admins need justification. Users have the least privilege principle—they get only what they need. Not “maybe later.”
At the same time, enforce multi-factor authentication (MFA) for all admin and clinical user accounts. Also, disable default accounts and change default passwords.
✅ Audit logs that actually work
Log every access to PHI: who, what, when, and where, including failed login attempts and permission changes. According to the HIPAA software compliance checklist, they should be stored securely for at least 6 years.
Still, logs are useless if you can’t search them. So build queryable audit trails early. Don’t wait until someone asks, “Did User X view Patient Y’s records on Tuesday?” and you’re grepping through terabytes of unstructured JSON.
✅ Do risk analysis
HIPAA requires an ongoing documented risk analysis. You have to identify and prevent threats before they happen. For example, could this database be leaked? Could someone spoof a user?
The document on how you’re mitigating each risk doesn’t have to be more than one hundred pages, but it should exist. Doing this helps prioritize security work without sounding alarmist.
✅ Check third-party vendors
Not all “secure” platforms are compliant out of the box. Using Twilio for SMS alerts with appointment details? They need to sign a BAA. Leveraging Firebase, Auth0, or S3? Check if they’re HIPAA-ready and willing to sign a BAA.
✅ Have a breach response plan
What if the worst case already happened and your data got exposed? Software HIPAA compliance checklist requires a clear plan.
- Do you know how to detect it?
- Who do you notify within 60 days? Patients? HHS?
- Is there a playbook?
To stay prepared, run a tabletop exercise once a year. It feels fake until it happens and then it’s terrifying.
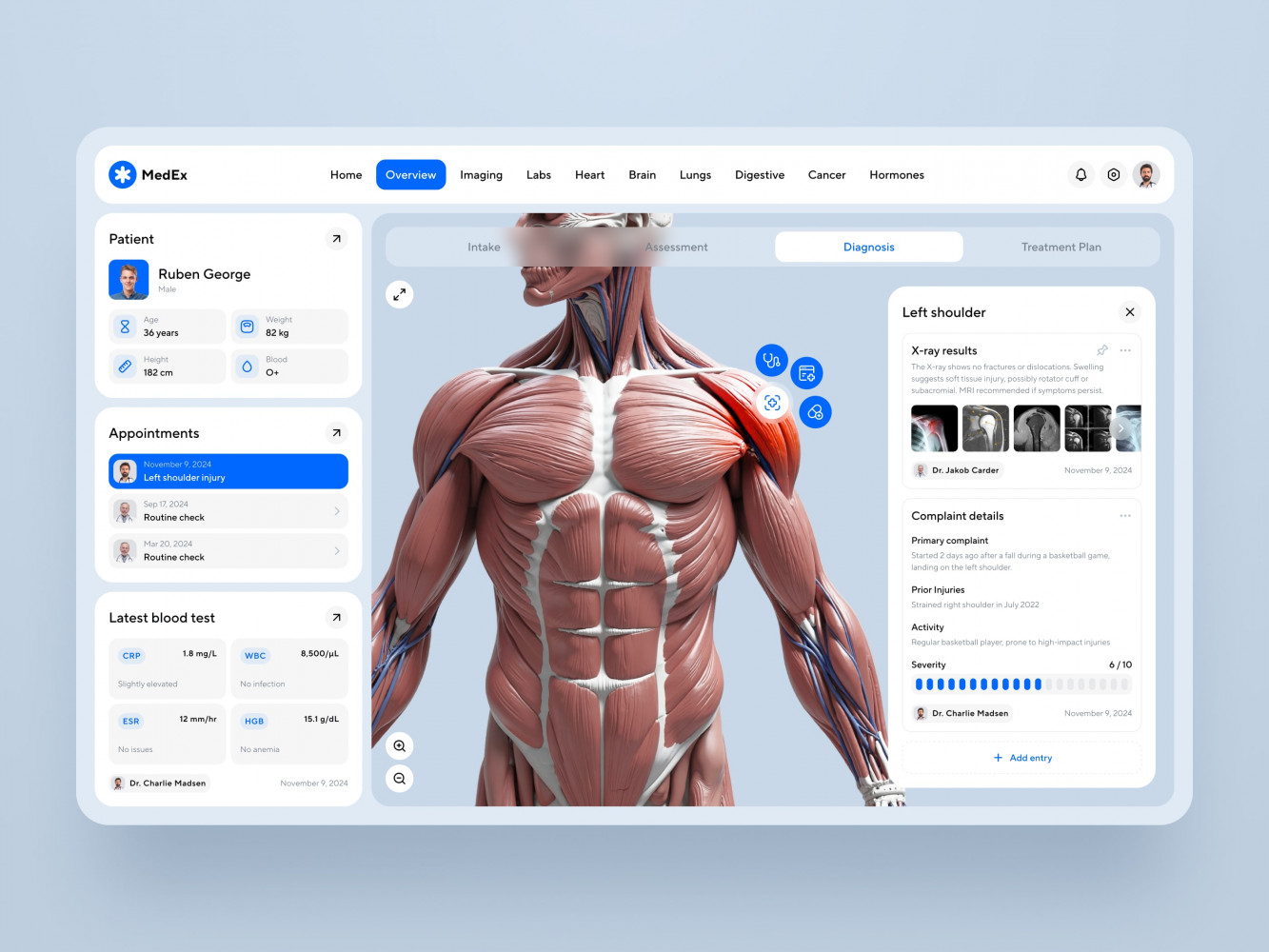
Medical Practice Management Software Dashboard Design by Shakuro
HIPAA Requirements for Software Development Teams
Your product touches PHI; what do you do now? What exactly should you keep in mind? There are many requirements, and I’ll split them into four sections for your convenience.
Let’s start with something you’re familiar with as a developer.
The Core: Technical Safeguards
These are the things you can actually code, configure, or design around.
Access control
HIPAA compliance for software development limits access to PHI to only authorized people.
- Implement strong authentication: MFA for all admin and clinical roles.
- Use role-based access control (RBAC): Billing clerk doesn’t need to read therapy notes.
- Auto-logout inactive sessions: Good call, especially on shared devices.
Encryption
It should be applied in both ways. TLS 1.2+ for transit with no exceptions, even for internal microservices. AES-256 is standard for encrypting data at rest: databases, backups, file storage, etc. The same goes for environment staging.
And don’t store keys in config files or GitHub. Instead, use key management services like KMS, Hashicorp Vault, etc.
Audit logs
Every time someone accesses PHI, you have to log it, writing their user ID, timestamp, action (view, edit, delete), patient ID, etc. These logs should be append-only and stored in a secured place. Again, like I said, retain them for at least six years, it’s a rule.
At the same time, make them searchable, where you can send a query and find a certain user or log. Because when there’s a breach or just a curious employee snooping, that’s the first thing you will do—check the logs.
Secure APIs & endpoints
The HIPAA-compliant software checklist requires authentication of every request with proper validation. Never expose PHI in URLs, error messages, or stack traces. Moreover, there should be a rate limit and monitoring for suspicious behavior. For example, when one user is pulling 500 records in a minute.
Integrity controls
If someone changes a medication dosage in the system, can you prove who did it and when? That’s a rather dangerous question. That’s why you need to eliminate any possibilities to alter or destroy the data improperly. For instance, you can use checksums or hashes to detect tampering.
Administrative Stuff
Yeah, some regulations are related to other stuff than code. You have to know them as well, even if you are a developer.
Risk analysis & management
As the one who writes code, you know where the data flows. So you know the risks. Where could PHI be exposed? What’s the likelihood? How bad would it be? Together with managers, you need to create an ongoing documented risk analysis. This will help you mitigate risks, fix misconfigurations, patch systems, and improve logging.
Workforce training
Everyone on the team needs basic knowledge about HIPAA compliance for software development. I don’t mean legal stuff where everyone turns into a lawyer, just some basics like “Don’t screenshot patient data. Don’t share logins. Report suspicious activity.” This includes engineers, QA, support, and even designers if they see real data.
BAAs with subcontractors
If you use third-party services, their providers have to be HIPAA compliant and sign a BAA with you.
Firebase, for example, supports HIPAA but only if you enable it and sign the BAA. Otherwise, you’re on your own.
Physical Safeguards
Third-party services
Most teams use cloud providers, so physical security is mostly handled for you. But still, if you have laptops with local databases, you need to encrypt them using tools like FileVault, BitLocker, etc. I don’t mention the basic stuff like not leaving devices unattended in public places.
Breach notification
If PHI is exposed, hacked, lost, or emailed to the wrong person, you may have to:
- Notify affected individuals.
- Report to HHS (Department of Health and Human Services).
- In some cases, notify the media.
There’s a 60-day window. So you need a plan before it happens.
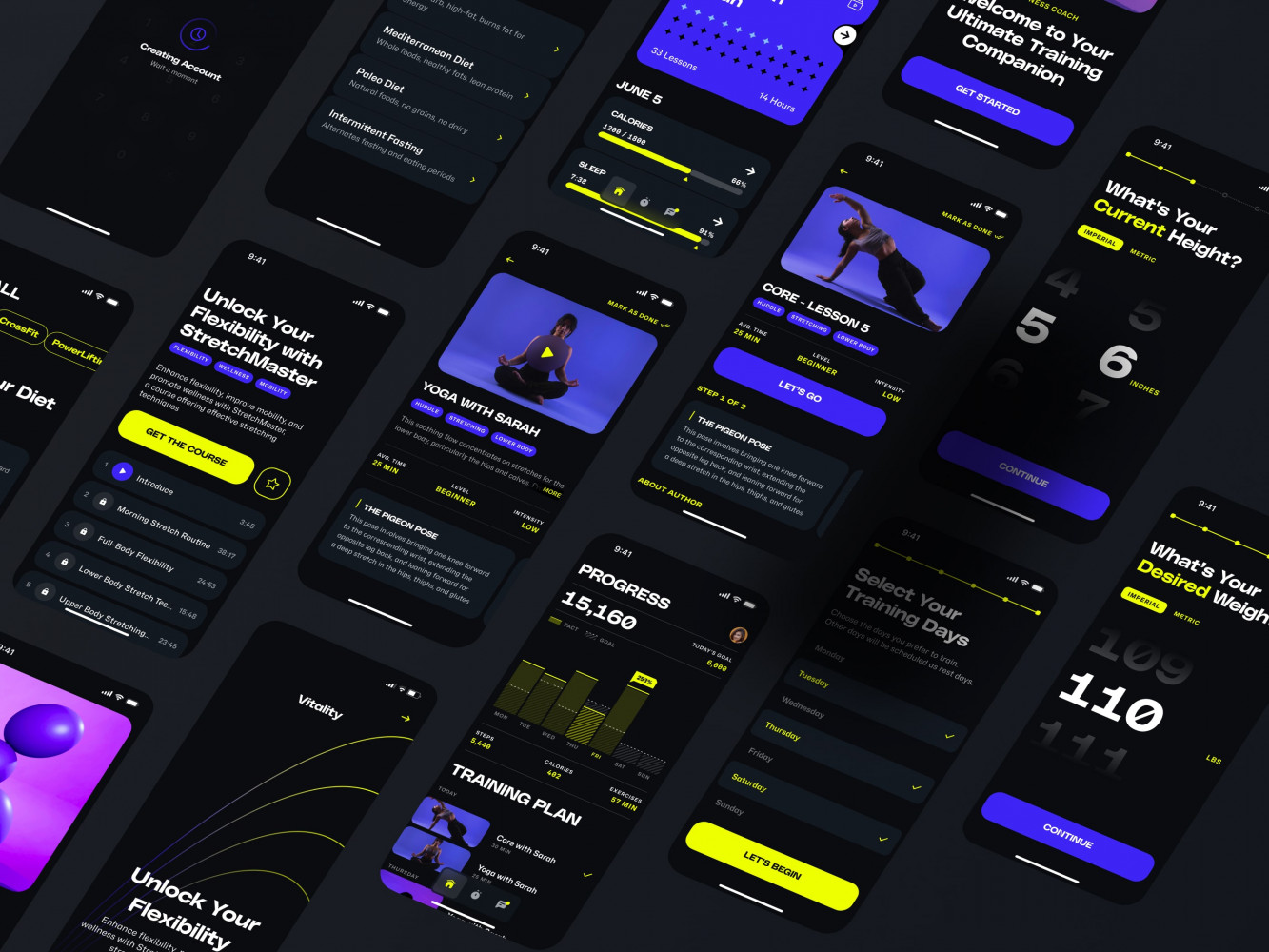
Mobile App Design for an Adaptive Fitness Guide by Shakuro
Common Mistakes That Lead to Non-Compliance
When following HIPAA compliant software requirements, it’s easy to take a wrong step. Here are some very common mistakes businesses make when they face this type of compliance.
❌ Handling PHI
This is the classic case when people don’t know they are related to PHI. For instance, a team builds a scheduling app. “We only store names and times,” they say. “No diagnoses!” But the appointment type is follow-up, or the clinic syncing the data is clearly a healthcare provider. And boom, they’ve got identifiers + health context = PHI.
HIPAA doesn’t care if you think it’s safe, it cares if it is. So when in doubt, treat it like PHI. It is easier than explaining yourself later.
❌Copying production data to staging
“Let’s pull last week’s data so QA can test properly.” I’ve seen teams dump full production databases into dev environments with real patient names, SSNs, and treatment notes because “it was easier for testing.”
The thing is, a staging server can have weak passwords and get scraped in a bot sweep. That’s a minor breach, which is still reportable and embarrassing.
To avoid that, use synthetic or de-identified data for testing. Or at minimum, scrub PHI before export.
❌ Logging too much or the wrong way
Logs are great until they leak PHI.
Common sins according to the HIPAA software compliance checklist:
- Error logs that dump full request bodies, including patient data.
- Debug mode left on in production.
- Stack traces showing database queries with names and IDs.
- Logs stored in unsecured cloud buckets or third-party tools.
What to do? Well, never log full PHI. Instead, mask or omit sensitive fields and secure your log storage like it’s a database.
❌ Skipping the BAA because “They’ll sign it later”
“We have a verbal agreement.”
“They said they’d get back to legal.”
“It’s just a pilot.”
Nope. If you’re processing PHI for a healthcare org and there’s no signed Business Associate Agreement, you’re non-compliant. The compliance officer will just shut it down cold, and months of work will get wasted.
So sign the BAA before data flows, not after or “soon.”
❌ Ignoring audit trails or building fake ones
Some teams slap together a “last accessed” timestamp and call it an audit log.
But the HIPAA compliance checklist for information technology wants more:
- Who accessed what?
- When?
- What did they do (view, edit, delete)?
- Was it successful?
And can you prove the log hasn’t been tampered with? For example, without proper protection, when audit logs live in the same database as the data itself, they can be deleted by the same admin role. Audit logs need to be immutable, protected, and separate enough that one compromised account can’t erase its tracks.
❌ Adding MFA later
Admin accounts, superusers, and backend access—these should all require MFA. This prevents unauthorized access and saves your data. You can use TOTP or WebAuthn, for example.
❌ Letting developers debug with real data
“This bug only happens in prod,” says the dev. So they pull raw records and paste them into Slack. Now there’s PHI in chat logs, on personal devices, possibly backed up to some SaaS tool with no BAA. Yes, I mentioned a similar situation with testers. Both are dangerous when you use raw data for completing tasks.
Instead, build safe debugging tools, redacted data views, feature flags, and local mocking.
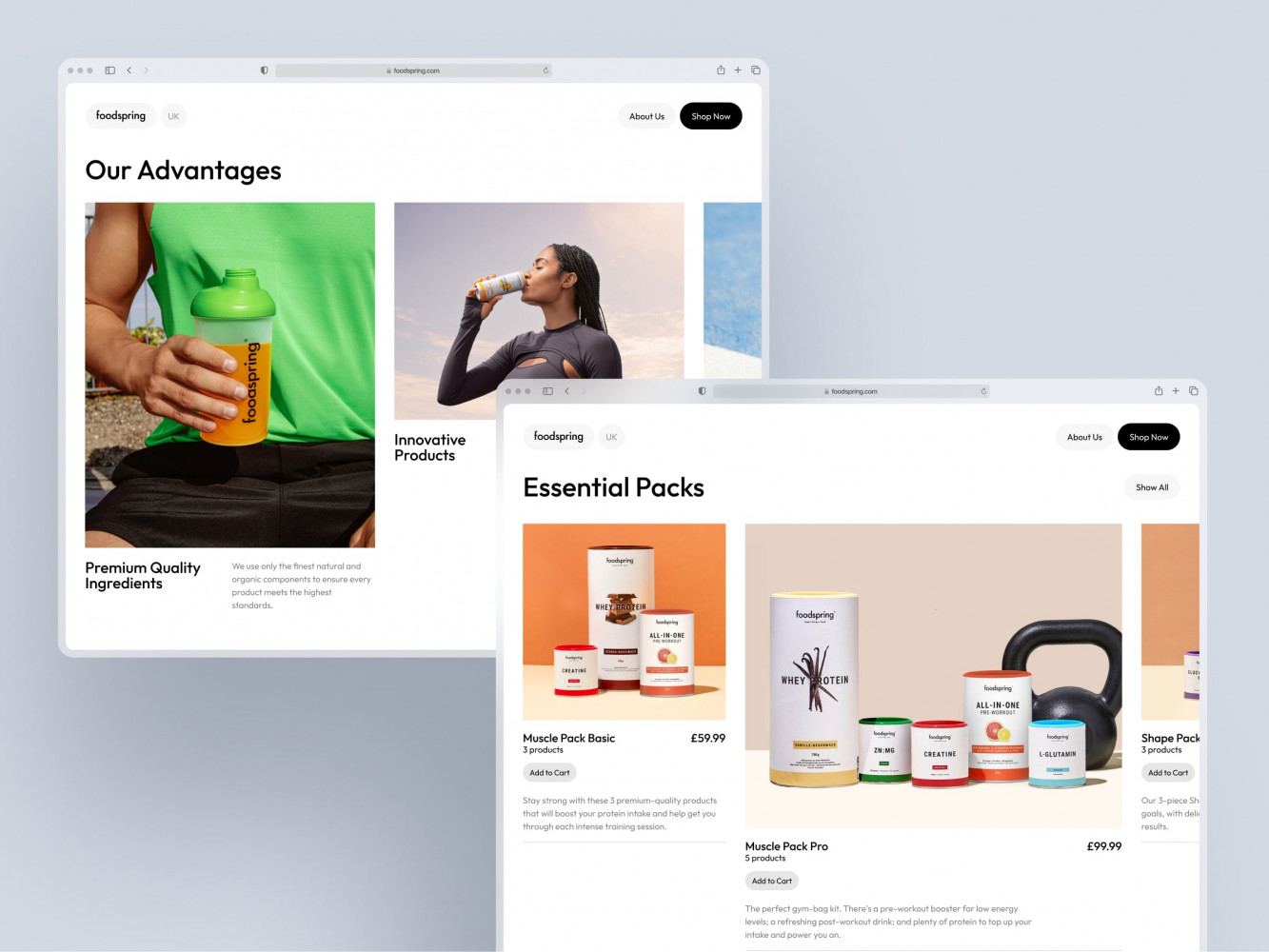
Web Design for a Supplements and Accessories Brand by Conceptzilla
How to Maintain HIPAA Compliance Throughout the Software Lifecycle
Another question: well, how do you make sure you don’t slip and become non-compliant while developing your healthcare app? Development is a complex process, and it’s easy to miss something.
Here are a few tips for you to adhere to HIPAA software compliance.
Design & Planning
Most compliance problems are born long before code is written. When you create your business idea and feature roadmap, you can see the areas touching PHI.
So, during this process, you need to ask several questions:
- Will this feature touch PHI?
- Can we avoid storing it? Minimize it?
- What access controls will it need?
- Should audit logging be built in from day one?
Quite often, startuppers think they will tack on privacy later, when they have time. But they won’t until a compliance officer comes knocking at their door, let’s be honest.
Development & QA
Along with planning, there are some practices you need to implement in the creation process. I’ve already mentioned some of them earlier when discussing the software HIPAA compliance checklist, but repetition is the mother of learning.
✅ Use secure defaults
- Force HTTPS in config.
- Encrypt database fields automatically (via ORM hooks or middleware).
- Reject unauthenticated API calls by default.
✅ Automate what you can
- Static analysis tools (like SonarQube, Snyk) can flag hardcoded secrets or weak crypto.
- Pre-commit hooks that block files containing “patient.ssn” or similar patterns.
- CI pipeline checks for missing MFA enforcement or unencrypted buckets.
✅ Test with realistic but safe data
Never use raw production data in dev or QA. Either generate synthetic PHI-like data (tools like Mockaroo can help) or properly de-identify real data: remove direct identifiers and shuffle dates. And train QA folks: “If you see real names in the UI during testing, stop and report it.”
Deployment
You’re deploying a new release—that’s exciting but risky, because there are several common pitfalls, like misconfigurations.
So:
- Use infrastructure-as-code (Terraform, CloudFormation) with security policies baked in.
- Scan deployments for open ports, weak encryption settings, or missing audit trails.
- Run compliance checks as part of your deployment gate.
Also, change management matters. HIPAA software compliance requires storing records of what changed, why, and who approved it. When auditors come, they will check that stuff.
Monitoring & Incident Response
Once it’s live, you need eyes on the system. Set up alerts for red flags:
- Unusual login times (e.g., an admin accessing data at 3 a.m. from a new country).
- Bulk downloads of patient records.
- Failed authentication spikes (possible brute force).
Logs should feed into a secure, access-controlled system, preferably with tamper protection. Additionally, have a plan in case things go south. For example, who gets paged if PHI is exposed? When it happens for real, you won’t have time to figure out roles. So run drills and see how fast you respond.
Ongoing Maintenance
Most teams stop here, which is a mistake. The process should never stop because trends change, preferences shift, people leave, vendors update, and threats evolve.
So, you need to review your risk analysis regularly: annually or after major changes. When contracts renew, BAAs should be prolonged along with them. Keep an eye on the patch systems and retrain your team to benefit from new hires, role changes, and refresher sessions.
With ongoing maintenance, you keep your app up-to-date with the latest trends and stay compliant with healthcare standards at the same time.
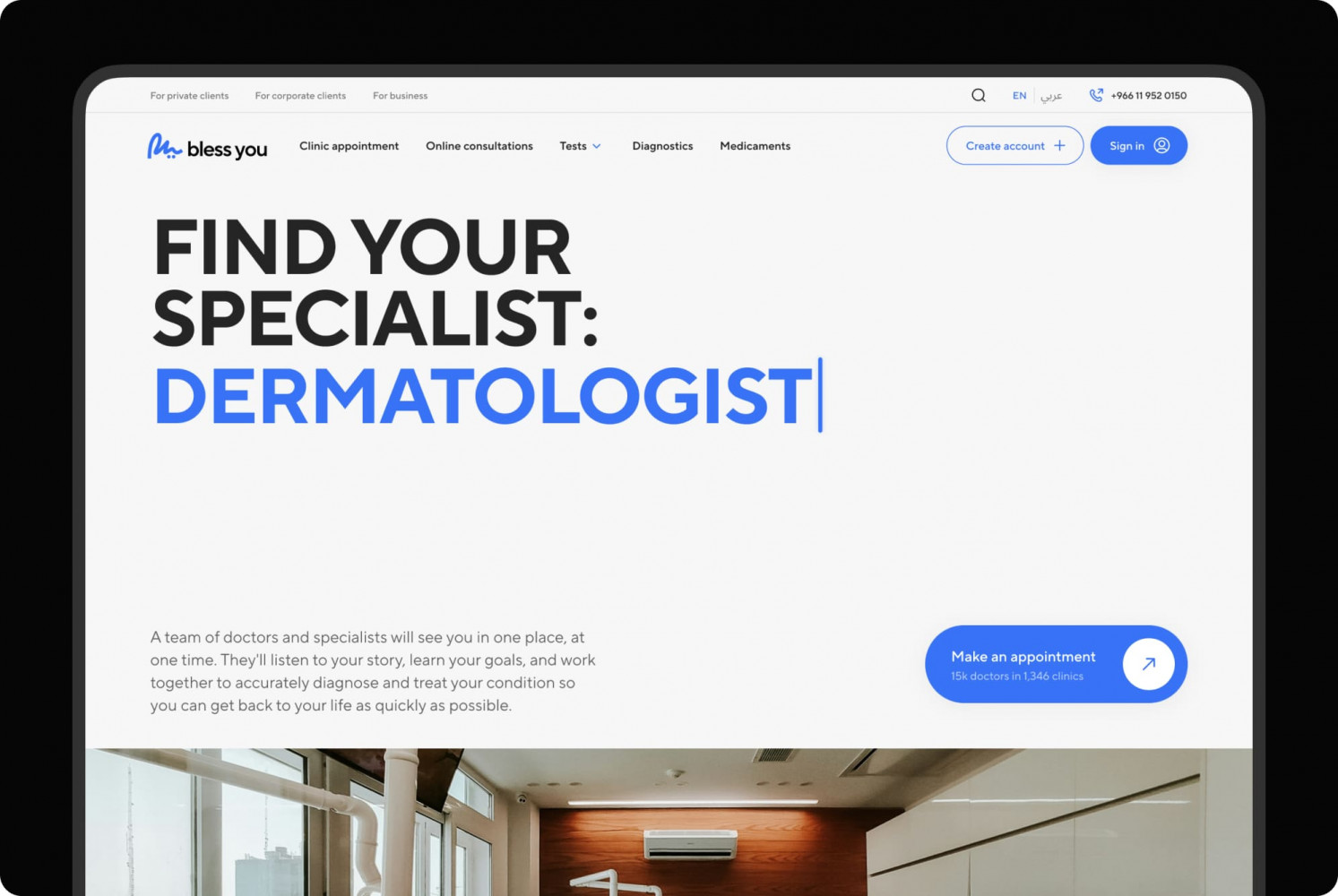
Bless You healthcare platform by Shakuro
HIPAA Compliance Resources for Developers
All these things can easily slip your mind. No wonder—there are regulations for devs, managers, and even stakeholders. Here’s a software HIPAA compliance checklist: official sources, practical tools, training, and frameworks you can actually integrate into your workflow.
🏛️ Official Guidance
HHS is the official hub. It may be a bit boring and authoritative, but it has all the essentials you need to know.
Key sections:
- HIPAA for Developers: A short page, basic but clear. Good for onboarding new team members.
- Security Rule Summary: Technical safeguards laid out plainly.
- Breach Notification Rule: Know when and how you must report.
There is also the OCR Breach Portal that shows what kinds of breaches get reported with real-world examples. Worth checking out to see the numbers.
NIST Special Publication 800-66 Rev. 2 is a cybersecurity resource guide created by the National Institute of Standards and Technology. It’s more structured, practical, and tech-friendly. The document breaks down each requirement with implementation suggestions, so you can use it as a reference when writing internal security policies.
🔧 Trusted Frameworks & Tools
HITRUST CSF is a unifying framework that maps HIPAA, NIST, ISO, and others into one actionable set of controls. It is widely adopted in healthcare, and some clients even require it. The certification is expensive and intense, though.
As a developer, you can use certain categories as a HIPAA compliant software checklist, even if you’re not getting certified.
SOC 2 Type II + HIPAA combination is a trust standard, as many healthcare customers ask for both. SOC 2 focuses on security, availability, and confidentiality. Together with HIPAA, you cover most bases.
OWASP ASVS (Application Security Verification Standard) is not exactly HIPAA-specific, but gold for secure software development. Some sections, like Error Handling and Logging, directly overlap with HIPAA technical safeguards. So you can run your code reviews against these levels.
☁️ Cloud Provider Compliance Docs
If you’re using AWS, Azure, or Google Cloud, read their HIPAA pages.
They tell you which services are eligible, how to enable compliance mode (for instance, AWS Artifact for BAAs), and what you still need to handle.
Key links:
- AWS HIPAA Compliance: Rather detailed, they even list which services support it.
- Azure HIPAA: Integrates with Microsoft’s compliance manager.
- Google Cloud HIPAA: Describes the conditions in detail.
🎓 Training & Certifications
There is training for tech teams you can take to speed up the implementation process of HIPAA software compliance.
For example, Cybrary is a course with a free intro that covers basics without legalese. Alternatively, you can search for HIPAA compliance on Udemy, there are many decent options with an affordable price.
Leads and architects can take certifications, which are helpful for credibility.
- CHP (Certified HIPAA Professional) from HIPAA that covers the landscape well.
- CISSP is a broader infosec certification, but it includes privacy principles.
- CIPP/US is more legal-focused but useful if you work closely with compliance officers.
🛠️ Tools That Help
Instruments like Vanta, Drata, or SecureFrame automate compliance monitoring. They usually connect to your AWS, GitHub, Okta, etc., and track BAAs, generate policies, and flag misconfigurations. It’s a great choice for startups prepping for audit.
There are also open-source tools, such as:
- Open Policy Agent (OPA): Enforces config policies, like “all buckets must be private.”
- Terraform + Checkov: Scans IaC for HIPAA-relevant risks.
- Hashicorp Vault: Manages secrets securely—encryption keys, DB credentials, etc.
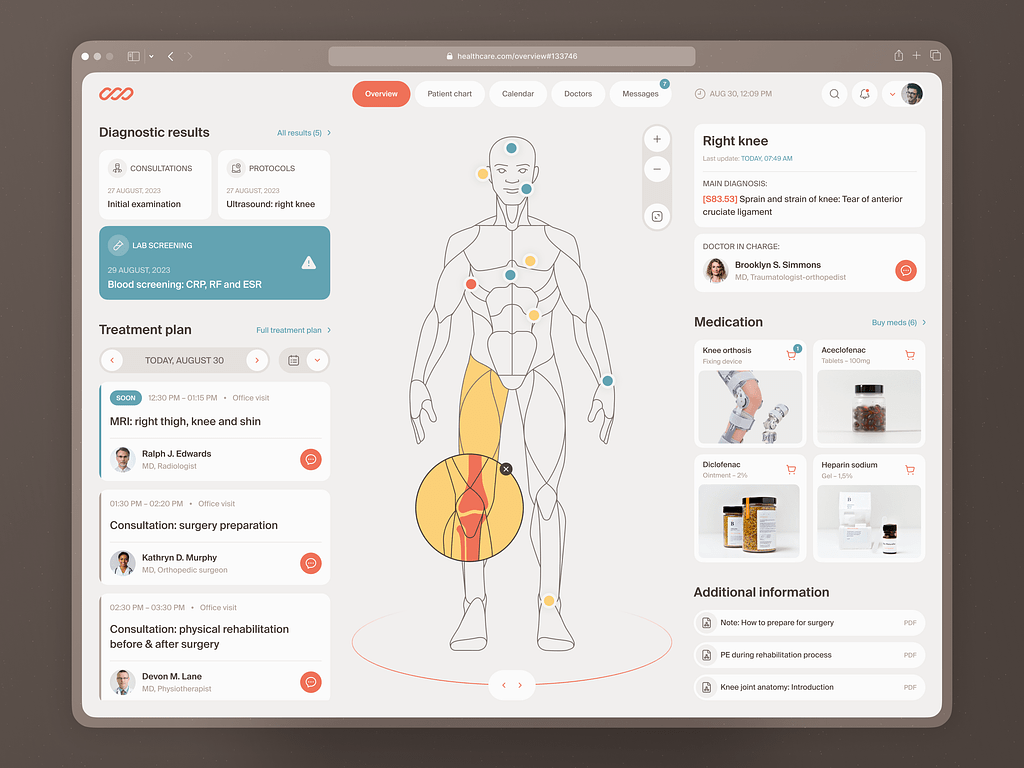
Medical Check-In Web Dashboard by Shakuro
Conclusion
HIPAA is one of the most important foundations you can build when developing healthcare software. We’ve covered a lot: spotting PHI in your data flow, encrypting at rest and in transit, logging access, signing BAAs, etc. But if you walk away with just a few things, make it these HIPAA compliant software requirements:
- Start early: Don’t treat HIPAA like a last-minute audit hurdle.
- Encrypt, control, log: Getting encryption right, locking down access, and keeping solid audit trails covers more than half the battle.
- Use the right tools and agreements: Make sure your stack supports compliance and that BAAs are signed before data moves.
- Train your team: Developers, product owners, QA—they all play a role.
- Keep it alive: Treat compliance like tech debt. Ignore it long enough, and it will come back to bite you.
Patients don’t see your elegant architecture or sleek UI. They care that their depression diagnosis doesn’t end up in a debug log. When you get it right, the software becomes more scalable, more credible, and easier to sell. You’re building something people can actually rely on.
